Peace be upon you!
Before you read this.
Smile with me and always keep praying with utmost faith.

What is depression?
Feeling down from time to time is a normal part of life, but when emotions such as hopelessness and despair take hold and just won’t go away, you may have depression. More than just sadness in response to life’s struggles and setbacks, depression changes how you think, feel, and function in daily activities. It can interfere with your ability to work, study, eat, sleep, and enjoy life. Just trying to get through the day can be overwhelming.
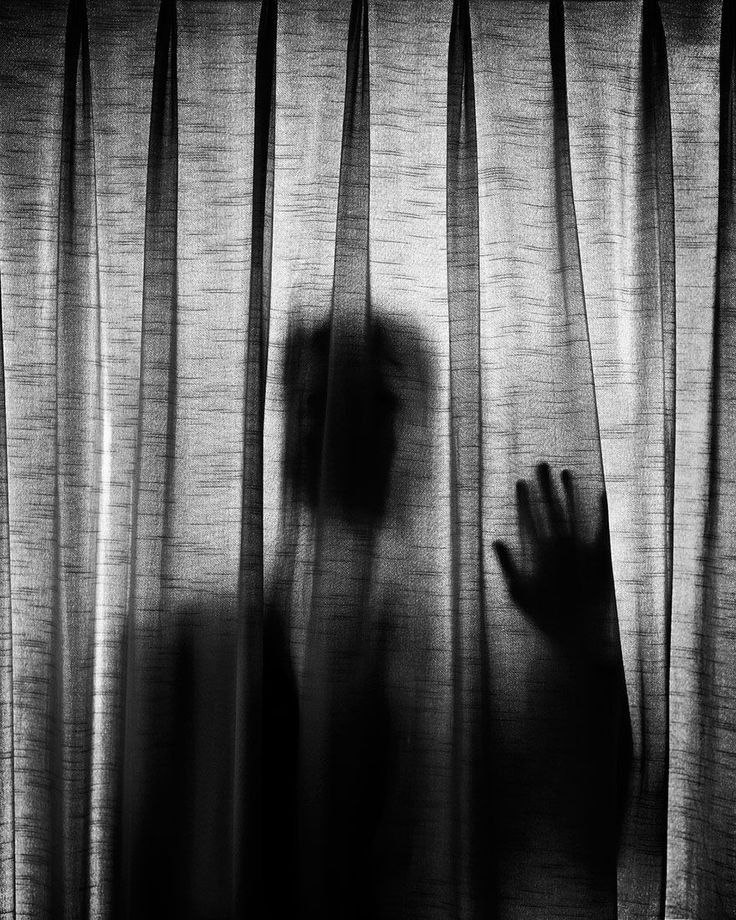
While some people describe depression as “living in a black hole” or having a feeling of impending doom, others feel lifeless, empty, and apathetic. Men in particular can feel angry and restless. However you experience the problem, left untreated it can become a serious health condition. But it’s important to remember that feelings of helplessness and hopelessness are symptoms of depression—not the reality of your situation.
No matter how hopeless you feel, you can get better. By understanding the causes and recognizing the different symptoms and types of depression, you can take the first steps to feeling better and overcoming the problem.
Signs and symptoms
Depression varies from person to person, but there are some common signs and symptoms. It’s important to remember that these symptoms can be part of life’s normal lows. But the more symptoms you have, the stronger they are, and the longer they’ve lasted—the more likely it is that you’re dealing with depression.
10 common depression symptoms
- Feelings of helplessness and hopelessness. A bleak outlook—nothing will ever get better and there’s nothing you can do to improve your situation.
- Loss of interest in daily activities. You don’t care anymore about former hobbies, pastimes, social activities, or sex. You’ve lost your ability to feel joy and pleasure.
- Appetite or weight changes. Significant weight loss or weight gain—a change of more than 5% of body weight in a month.
- Sleep changes. Either insomnia, especially waking in the early hours of the morning, or oversleeping.
- Anger or irritability. Feeling agitated, restless, or even violent. Your tolerance level is low, your temper short, and everything and everyone gets on your nerves.
- Loss of energy. Feeling fatigued, sluggish, and physically drained. Your whole body may feel heavy, and even small tasks are exhausting or take longer to complete.
- Self-loathing. Strong feelings of worthlessness or guilt. You harshly criticize yourself for perceived faults and mistakes.
- Reckless behavior. You engage in escapist behavior such as substance abuse, compulsive gambling, reckless driving, or dangerous sports.
- Concentration problems. Trouble focusing, making decisions, or remembering things.
- Unexplained aches and pains. An increase in physical complaints such as headaches, back pain, aching muscles, and stomach pain.

The link between depression symptoms and anxiety
Depression and anxiety are believed to stem from the same biological vulnerability, which may explain why they so often go hand-in-hand. Since anxiety makes depression worse (and vice versa), it’s important to seek treatment for both conditions.
Is it depression or bipolar disorder?
Bipolar disorder, also known as manic depression, involves serious shifts in moods, energy, thinking, and behavior. Because it looks so similar to depression when in the low phase, it is often overlooked and misdiagnosed.
This can be a serious problem as taking antidepressants for bipolar disorder can actually make the condition worse. If you’ve ever gone through phases where you experienced excessive feelings of euphoria, a decreased need for sleep, racing thoughts, and impulsive behavior, consider getting evaluated for bipolar disorder.
[Read: Bipolar Disorder Signs and Symptoms]
Depression and suicide risk
Depression is a major risk factor for suicide. Deep despair and hopelessness can make suicide feel like the only way to escape the pain. If you have a loved one with depression, take any suicidal talk or behavior seriously and watch for the warning signs:
- Talking about killing or harming one’s self.
- Expressing strong feelings of hopelessness or being trapped.
- An unusual preoccupation with death or dying.
- Acting recklessly, as if they have a death wish (e.g. speeding through red lights).
- Calling or visiting people to say goodbye.
- Getting affairs in order (giving away prized possessions, tying up loose ends).
- Saying things like “Everyone would be better off without me,” or “I want out.”
- A sudden switch from being extremely down to acting calm and happy.
If you think a friend or family member is considering suicide, express your concern and seek help immediately. Talking openly about suicidal thoughts and feelings can save a life.

How depression symptoms vary with gender and age
Depression often varies according to age and gender, with symptoms differing between men and women, or young people and older adults.
Men
Depressed men are less likely to acknowledge feelings of self-loathing and hopelessness. Instead, they tend to complain about fatigue, irritability, sleep problems, and loss of interest in work and hobbies. They’re also more likely to experience symptoms such as anger, aggression, reckless behavior, and substance abuse.
Women
Women are more likely to experience symptoms such as pronounced feelings of guilt, excessive sleeping, overeating, and weight gain. Depression in women is also impacted by hormonal factors during menstruation, pregnancy, and menopause. In fact, postpartum depression affects up to 1 in 7 women following childbirth.
Teens
Irritability, anger, and agitation are often the most noticeable symptoms in depressed teens—not sadness. They may also complain of headaches, stomachaches, or other physical pains.
Older adults
Older adults tend to complain more about the physical rather than the emotional signs and symptoms: things like fatigue, unexplained aches and pains, and memory problems. They may also neglect their personal appearance and stop taking critical medications for their health.
Types of depression
Depression comes in many shapes and forms. While defining the severity—whether it’s mild, moderate, or major—can be complicated, knowing what type you have may help you manage your symptoms and get the most effective treatment.
Mild and moderate depression
These are the most common types. More than simply feeling blue, the symptoms of mild depression can interfere with your daily life, robbing you of joy and motivation. Those symptoms become amplified in moderate depression and can lead to a decline in confidence and self-esteem.
Recurrent, mild depression (dysthymia)
Dysthymia is a type of chronic “low-grade” depression. More days than not, you feel mildly or moderately depressed, although you may have brief periods of normal mood.
- The symptoms of dysthymia are not as strong as the symptoms of major depression, but they last a long time (at least two years).
- Some people also experience major depressive episodes on top of dysthymia, a condition known as “double depression.”
- If you suffer from dysthymia, you may feel like you’ve always been depressed. Or you may think that your continuous low mood is “just the way you are.”
Major or clinical depression
Major depression (otherwise known as major depressive disorder) is much less common than mild or moderate and is characterized by severe, relentless symptoms.
- Left untreated, major depressive disorder typically lasts for about six months.
- Some people experience just a single depressive episode in their lifetime, but major depression can be a recurring disorder.
Atypical depression
Atypical depression is a common subtype of major depressive disorder with a specific symptom pattern. It responds better to some therapies and medications than others, so identifying it can be helpful.
- People with atypical depression experience a temporary mood lift in response to positive events, such as after receiving good news or while out with friends.
- Other symptoms include weight gain, increased appetite, sleeping excessively, a heavy feeling in the arms and legs, and sensitivity to rejection.
Seasonal affective disorder (SAD)
For some people, the reduced daylight hours of winter lead to a form of depression known as seasonal affective disorder (SAD). SAD affects about 1% to 2% of the population, particularly women and young people. SAD can make you feel like a completely different person to who you are in the summer: hopeless, sad, tense, or stressed, with no interest in friends or activities you normally love. SAD usually begins in fall or winter when the days become shorter and remains until the brighter days of spring.
Causes and risk factors.
While some illnesses have a specific medical cause, making treatment straightforward, depression is far more complicated. Certain medications, such as barbiturates, corticosteroids, benzodiazepines, opioid painkillers, and specific blood pressure medicine can trigger symptoms in some people—as can hypothyroidism (an underactive thyroid gland). But most commonly, depression is caused by a combination of biological, psychological, and social factors that can vary wildly from one person to another.
Despite what you may have seen in TV ads, read in newspaper articles, or maybe even heard from a doctor, depression is not just the result of a chemical imbalance in the brain, having too much or too little of any brain chemical that can be simply cured with medication. Biological factors can certainly play a role in depression, including inflammation, hormonal changes, immune system suppression, abnormal activity in certain parts of the brain, nutritional deficiencies, and shrinking brain cells. But psychological and social factors—such as past trauma, substance abuse, loneliness, low self-esteem, and lifestyle choices—can also play an enormous part.
Risk factors that can make you more vulnerable
Depression most often results from a combination of factors, rather than one single cause. For example, if you went through a divorce, were diagnosed with a serious medical condition, or lost your job, the stress could prompt you to start drinking more, which in turn could cause you to withdraw from family and friends. Those factors combined could then trigger depression.
The following are examples of risk factors that can make you more susceptible:
Loneliness and isolation. There’s a strong relationship between loneliness and depression. Not only can lack of social support heighten your risk, but having depression can cause you to withdraw from others, exacerbating feelings of isolation. Having close friends or family to talk to can help you maintain perspective on your issues and avoid having to deal with problems alone.
Marital or relationship problems. While a network of strong and supportive relationships can be crucial to good mental health, troubled, unhappy, or abusive relationships can have the opposite effect and increase your risk for depression.
Recent stressful life experiences. Major life changes, such as a bereavement, divorce, unemployment, or financial problems can often bring overwhelming levels of stress and increase your risk of developing depression.
Chronic illness or pain. Unmanaged pain or being diagnosed with a serious illness, such as cancer, heart disease, or diabetes, can trigger feelings of hopelessness and helplessness.
Family history of depression. Since it can run in families, it’s likely some people have a genetic susceptibility to the problem. However, there is no single “depression” gene. And just because a close relative suffers from depression, it doesn’t mean you will, too. Your lifestyle choices, relationships, and coping skills matter just as much as genetics.
Personality. Whether your personality traits are inherited from your parents or the result of life experiences, they can impact your risk of depression. For example, you may be at a greater risk if you tend to worry excessively, have a negative outlook on life, are highly self-critical, or suffer from low self-esteem.
Early childhood trauma or abuse. Early life stresses such as childhood trauma, abuse, or bullying can make you more susceptible to a number of future health conditions, including depression.
Alcohol or drug abuse. Substance abuse can often co-occur with depression. Many people use alcohol or drugs as a means of self-medicating their moods or cope with stress or difficult emotions. If you are already at risk, abusing alcohol or drugs may push you over the edge. There is also evidence that those who abuse opioid painkillers are at greater risk for depression.
The cause of your depression may help determine the treatment
Understanding the underlying cause of your depression may help you overcome the problem. For example, if you are feeling depressed because of a dead-end job, the best treatment might be finding a more satisfying career rather than simply taking an antidepressant. If you are new to an area and feeling lonely and sad, finding new friends will probably give you more of a mood boost than going to therapy. In such cases, the depression is remedied by changing the situation.
Whether you’re able to isolate the causes or not, the most important thing is to recognize that you have a problem, reach out for support, and pursue the coping strategies that can help you to feel better.

10 Natural Depression Treatments
Being depressed can make you feel helpless. You’re not. Along with therapy and sometimes medication, there’s a lot you can do on your own to fight back. Changing your behavior — your physical activity, lifestyle, and even your way of thinking — are all natural depression treatments.
These tips can help you feel better — starting right now.
1. Get in a routine. If you’re depressed, you need a routine, says Ian Cook, MD. He’s a psychiatrist and director of the Depression Research and Clinic Program at UCLA.
Depression can strip away the structure from your life. One day melts into the next. Setting a gentle daily schedule can help you get back on track.
2.Set goals. When you’re depressed, you may feel like you can’t accomplish anything. That makes you feel worse about yourself. To push back, set daily goals for yourself.
“Start very small,” Cook says. “Make your goal something that you can succeed at, like doing the dishes every other day.”
As you start to feel better, you can add more challenging daily goals.
3. Exercise. It temporarily boosts feel-good chemicals called endorphins. It may also have long-term benefits for people with depression. Regular exercise seems to encourage the brain to rewire itself in positive ways, Cook says.
How much exercise do you need? You don’t need to run marathons to get a benefit. Just walking a few times a week can help.

4. Eat healthy. There is no magic diet that fixes depression. It’s a good idea to watch what you eat, though. If depression tends to make you overeat, getting in control of your eating will help you feel better.
Although nothing is definitive, Cook says there’s evidence that foods with omega-3 fatty acids (such as salmon and tuna) and folic acid (such as spinach and avocado) could help ease depression.
5. Get enough sleep. Depression can make it hard to get enough shut-eye, and too little sleep can make depression worse.
What can you do? Start by making some changes to your lifestyle. Go to bed and get up at the same time every day. Try not to nap. Take all the distractions out of your bedroom — no computer and no TV. In time, you may find your sleep improves.
6. Take on responsibilities. When you’re depressed, you may want to pull back from life and give up your responsibilities at home and at work. Don’t. Staying involved and having daily responsibilities can help you maintain a lifestyle that can help counter depression. They ground you and give you a sense of accomplishment.
If you’re not up to full-time school or work, that’s fine. Think about part-time. If that seems like too much, consider volunteer work.
7. Challenge negative thoughts. In your fight against depression, a lot of the work is mental — changing how you think. When you’re depressed, you leap to the worst possible conclusions.
The next time you’re feeling terrible about yourself, use logic as a natural depression treatment. You might feel like no one likes you, but is there real evidence for that? You might feel like the most worthless person on the planet, but is that really likely? It takes practice, but in time you can beat back those negative thoughts before they get out of control.
8. Check with your doctor before using supplements. “There’s promising evidence for certain supplements for depression,” Cook says. Those include fish oil, folic acid, and SAMe. But more research needs to be done before we’ll know for sure. Always check with your doctor before starting any supplement, especially if you’re already taking medications.
9. Do something new. When you’re depressed, you’re in a rut. Push yourself to do something different. Go to a museum. Pick up a used book and read it on a park bench. Volunteer at a soup kitchen. Take a language class.
“When we challenge ourselves to do something different, there are chemical changes in the brain,” Cook says. “Trying something new alters the levels of [the brain chemical] dopamine, which is associated with pleasure, enjoyment, and learning.”
10. Try to have fun. If you’re depressed, make time for things you enjoy. What if nothing seems fun anymore? “That’s just a symptom of depression,” Cook says. You have to keep trying anyway.
As strange as it might sound, you have to work at having fun. Plan things you used to enjoy, even if they feel like a chore. Keep going to the movies. Keep going out with friends for dinner.
When you’re depressed, you can lose the knack for enjoying life, Cook says. You have to relearn how to do it. In time, fun things really will feel fun again.
